


Analysis on Efficacy and Safety of Nano-knife Ablation in Treating Advanced Gallbladder Carcinoma was first published on the China National Knowledge Infrastructure (CNKI) website, citing some of the content in order to better inform readers about Nanoknife ablation therapy.
【Citation of literature】SHI Zhigang ,LI Xiaoyong ,CHEN Yanj un ,CHENG Bingbing , CHEN Sheng yang ,HU Shuiquan ,TONG Hao, Analysis on Efficacy and Safety of Nano-knife Ablation in Treating Advanced Gallbladder Carcinoma [J/OL].Chongqing Yingxue:1-9[2022-10-31].
http://kns.cnki.net/kcms/detail/50.1097.R.20220831.1112.002.html
Analysis on Efficacy and Safety of Nano-knife Ablation in Treating Advanced Gallbladder Carcinoma
Abstract
Objective : To analyze the efficacy and safety of nano-knife ablation in the treatment of advanced gallbladder carcinoma.
Methods : The clinical data of 3 6 patients with advanced gallbladder cancer treated in this hospital from October 20 1 6 to October 20 1 8 were collected.The patients receiving nano-knife ablation combined with percutaneous transhepaticcholangial drainage (PTCD,n =20)served as the study group, those only receiving PTCD as the as the control group (n = 1 6 ).The changes of serum total bilirubin and CA1 9-9,quality of life score,median survival time and complications occurrence at postoperative 2 weeks,1 and 2 months were compared between the two groups.
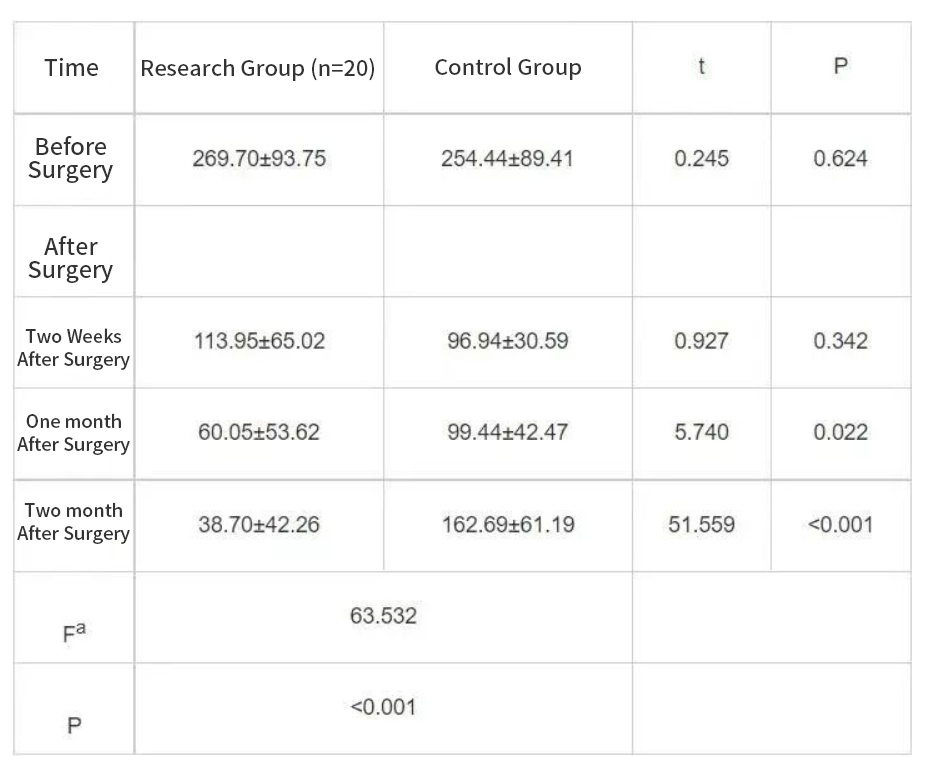
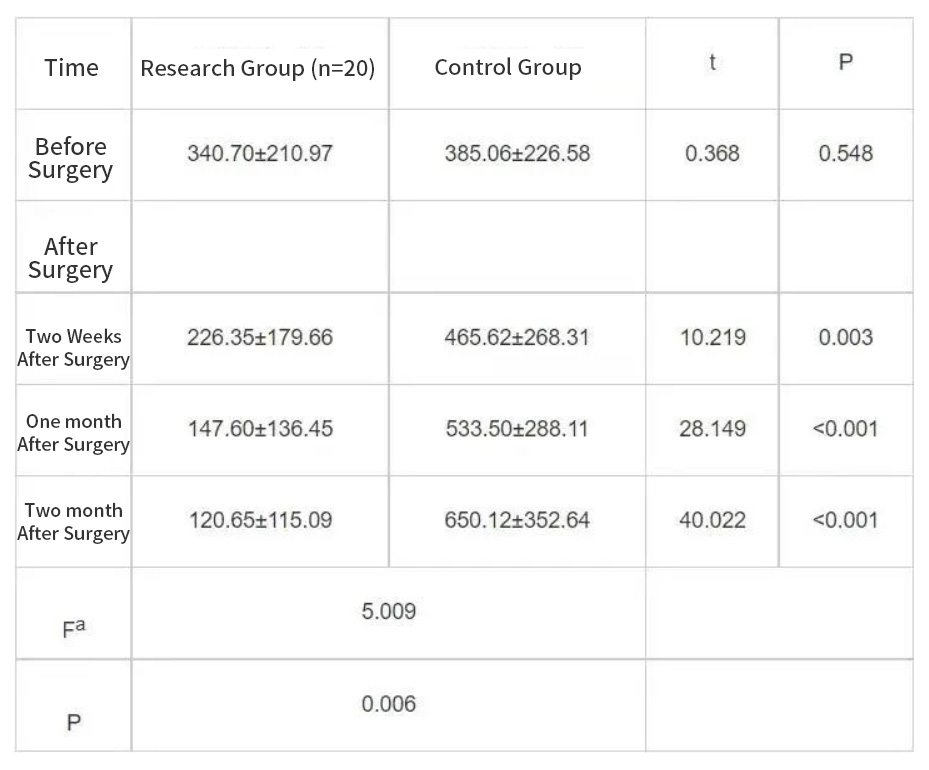
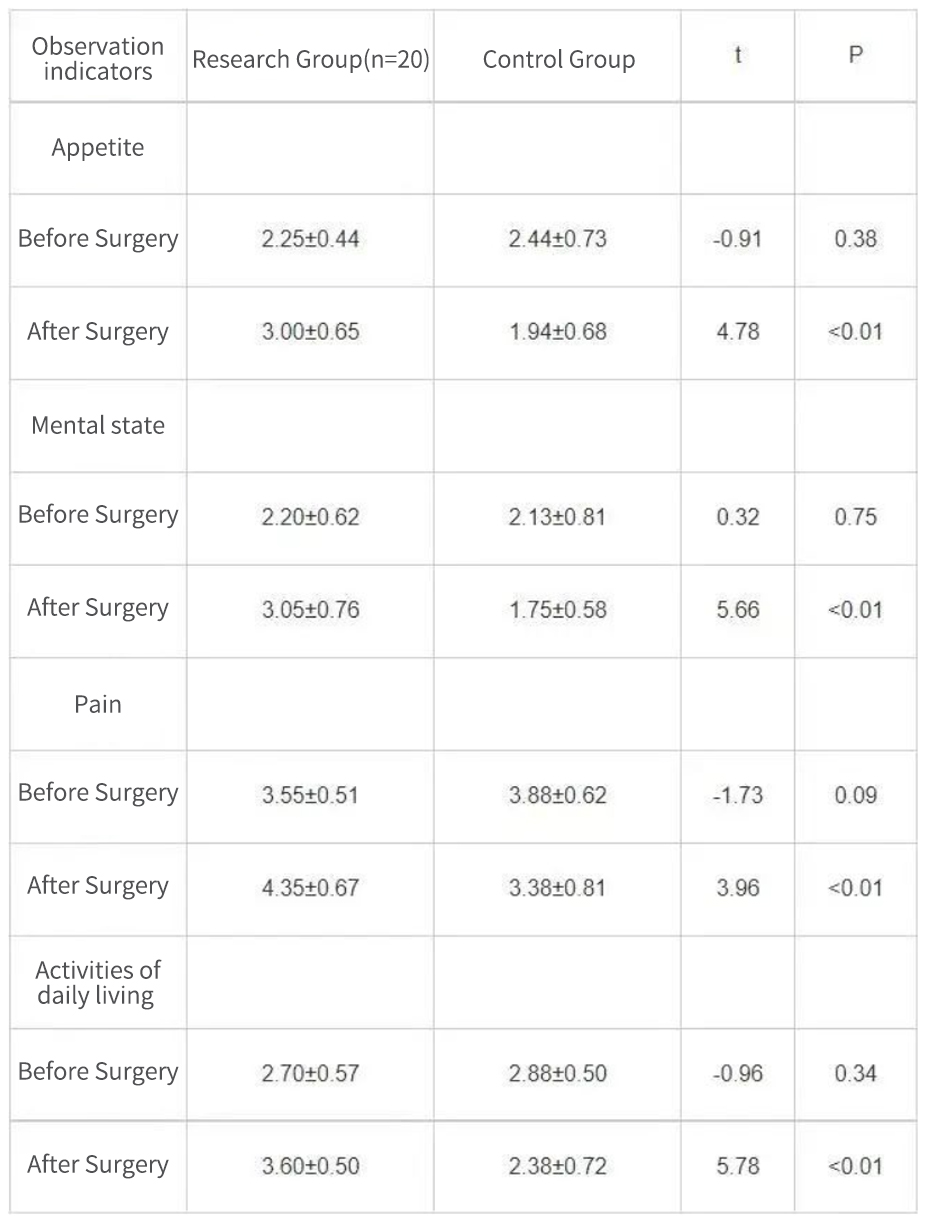
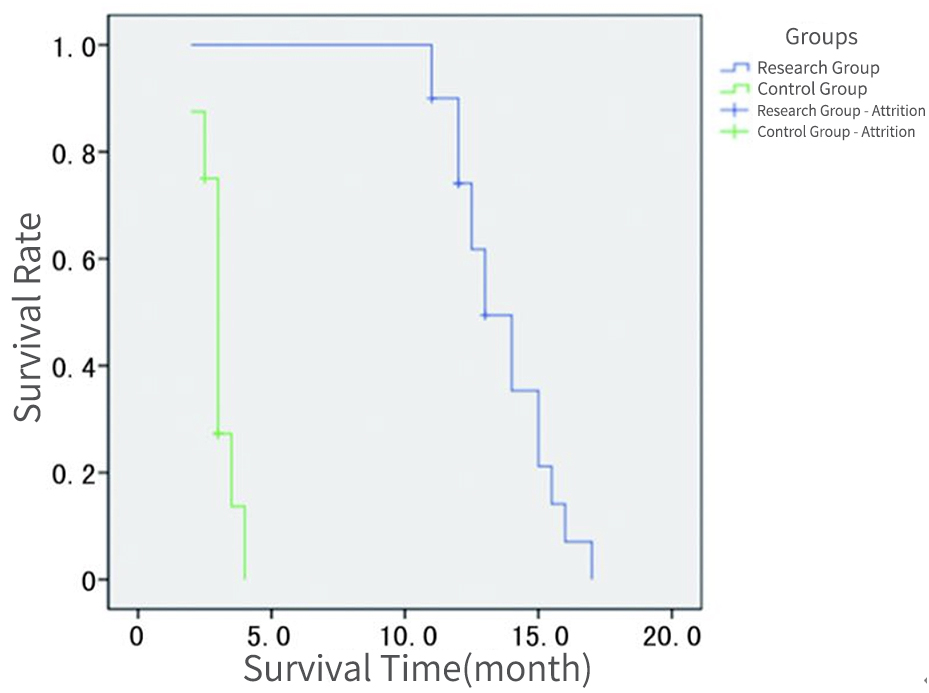
Results:There was no statistically significant difference in the levels of serum total bilirubin and CA1 9-9 before operation between the two groups (P >0.0 5).The levels of serum total bilirubin at postoperative 2 weeks,1 and 2 months in the two groups were decreased compared with those before operation,moreover,which at postoperative 1 and 2 months in the study group were significantly lower than those in the control group (P < 0.0 5 ).At postoperative 2 weeks,1 and 2 months,the level of serum CA1 9-9 in the study group was significantly lower than that before operation (P<0.0 5),while the level of serum CA1 9-9 in the control group was significantly higher than that before operation (P <0.0 5).There were statistically significant differences in serum CA1 9-9 levels at postoperative time points between the two groups (P <0.0 .there="" were="" no="" statistically="" significant="" difference="" in="" the="" scores="" of="" all="" dimensions="" quality="" life="" before="" operation="" between="" two="" groups="" p="">0.0 5),while the scores of all dimensions of quality of life at postoperative 2 months in the study group were significantly higher than those in the control group (P<0.0 5).The postoperative PTCD tube angiography showed that 1 9 cases in the study group achieved the biliary tract recanalization,with a recanalization rate of 9 5.0%.The median survival time in the study group was significantly longer than that in the control group (1 3 months vs .3 months,P <0.0 3="" 5="" .after="" there="" were="" one="" case="" of="" biliary="" tract="" liver="" abscess="" and="" gastrointestinal="" bleeding="" in="" the="" study="" total="" complications="" occurrence="" rate="" was="" cases="" bile="" infection="" control="" with="" a="" incidence="" .there="" no="" statistically="" significant="" difference="" between="" two="" groups="" p="">0.0 5).
Conclusion:Nanoknife ablation could prolong the survival time of the patients,improve their quality of life,and has high safety.Gallbladder cancer is the most common malignant tumor in the biliary system, ranking sixth in incidence among digestive system tumors. It has a high degree of malignancy and a poor prognosis, with a 5-year survival rate of only about 5%. When most patients present with clinical symptoms such as abdominal pain and jaundice, it often indicates that the disease is already in the advanced stage, with the tumor invading adjacent structures and organs (extrahepatic bile ducts, liver, stomach, colon, etc.) or distant metastasis and lymphatic metastasis have occurred. Among them, for patients without distant metastasis, with obstruction jaundice caused by invasion of the hepatic bile duct and blood vessels, radical surgical treatment can be performed, but the risk is extremely high and should be carried out with caution; while patients with distant metastasis have no chance of radical surgical treatment.
Irreversible electroporation (IRE), also known as Nanoknife, uses high-voltage electric pulses to create multiple irreversible nanoscale pores in the tumor cell membrane, disrupting the cell's internal balance and ultimately causing rapid apoptosis of the tumor cells without damaging adjacent structures such as blood vessels and bile ducts. In recent years, Nanoknife has gradually been applied to the treatment of locally advanced pancreatic cancer and hilar cholangiocarcinoma due to its high safety and low postoperative complications, and can significantly improve patient prognosis, but its efficacy in advanced gallbladder cancer is not yet clear. This study retrospectively analyzed the clinical data of 20 patients with advanced gallbladder cancer who underwent Nanoknife ablation at our hospital from October 2016 to October 2018, summarized the postoperative complications and survival indicators of the patients, in order to provide more clinical ideas for the treatment of advanced gallbladder cancer.
Research results
Comparison of serological indicators between two groups of patients.
Comparison of preoperative total bilirubin levels between two groups of patients showed no statistically significant difference (P>0.05). However, the postoperative total bilirubin levels of both groups were significantly reduced at 2 weeks, 1 month, and 2 months after surgery (P<0.05), 1="" 2="" with="" the="" control="" group="" showing="" an="" increase="" in="" total="" bilirubin="" levels="" at="" months="" after="" surgery="" compared="" to="" month="" surgery.="" there="" was="" no="" significant="" difference="" between="" two="" groups="" weeks="" p="">0.05), but the postoperative total bilirubin levels of the study group were significantly lower than those of the control group at 1 and 2 months after surgery (P<0.05).
Comparison of preoperative serum CA19-9 levels between two groups of patients showed no statistically significant difference (P>0.05). However, the postoperative serum CA19-9 levels of the study group were significantly reduced at 2 weeks, 1 month, and 2 months after surgery (P<0.05), while the control group showed a continuous increase in serum CA19-9 levels at the same time points after surgery (P<0.05). The difference in serum CA19-9 levels between the two groups at each time point after surgery was statistically significant (P<0.05).
Comparison of quality of life scores between two groups of patients.
According to the quality of life score scale for cancer patients, there was no statistically significant difference (P>0.05) in the scores of each dimension of quality of life between the two groups of patients before surgery. However, two months after surgery, the scores of each dimension of quality of life in the study group were higher than those in the control group, and the difference was statistically significant (P<0.05).
The bile duct patency and median survival time of the two patient groups.
The study compared the bile duct patency and median survival time of two groups of patients. The research group underwent PTCD for bile duct imaging after surgery, and the results showed that 19 patients had bile duct patency, with a patency rate of 95.0%, and the postoperative patency time was (161.7±51.5) days. All 19 patients had their PTCD tubes removed after 3 months. The control group had a postoperative patency time of (52.1±10.8) days. The difference in postoperative patency time between the two groups was statistically significant (P<0.05). The median survival time of the research group was 13 months, with the longest survival time being 17 months and the shortest being 11 months. The median survival time of the control group was 3 months, with the longest survival time being 4 months and the shortest being 2 months. The median survival time of the research group was significantly higher than that of the control group (P<0.05).
Discussion
In recent years, Nanoknife ablation has been applied in the treatment of locally advanced pancreatic cancer and hilar cholangiocarcinoma, as it can ablate tumors without significantly affecting surrounding connective tissue and collagen, thus protecting structures such as blood vessels or bile ducts that are invaded by tumors. In terms of the efficacy of Nanoknife ablation in this study, the postoperative serum total bilirubin levels of both groups of patients decreased compared to preoperative levels, and the levels in the study group were significantly lower than those in the control group at 1 and 2 months after surgery (P<0.05), showing a progressive decrease. However, the serum total bilirubin levels in the control group increased again at 2 months after surgery, possibly due to factors such as PTCD tube blockage, tumor progression, and poor liver function. The serum CA19-9 levels of the study group patients decreased at 2 weeks, 1 month, and 2 months after surgery compared to preoperative levels, indicating that Nanoknife ablation can effectively destroy tumor tissue. The serum CA19-9 levels in the control group patients continued to rise after surgery, and there was a significant difference in serum CA19-9 levels between the two groups at each time point after surgery (P<0.05). After PTCD tube cholangiography, the study group patients achieved bile duct patency in 19 cases, with a patency rate of 95.0%, similar to the bile duct patency rate after Nanoknife ablation for unresectable hilar cholangiocarcinoma. The patency time after surgery was (161.7±51.5) days, and all 19 patients had their PTCD tubes removed 3 months after surgery. The patency time in the control group was (52.1±10.8) days, and there was a significant difference in patency time between the two groups after surgery (P<0.05). In addition, the median survival time and postoperative quality of life score of the study group patients were higher than those of the control group, indicating that Nanoknife ablation can not only prolong the survival time of patients, but also create opportunities for patients to remove drainage tubes and improve their quality of life.
In conclusion, NanoKnife ablation can significantly damage tumor tissue, delay tumor progression, prolong patient survival, and achieve biliary patency, providing the possibility of removing PTCD tubes and avoiding the inconvenience caused by long-term drainage tubes, thereby improving the quality of life of patients. In addition, NanoKnife ablation has fewer complications and is highly safe. However, due to the small sample size of this study, further research is needed to analyze the efficacy of NanoKnife ablation in the treatment of advanced gallbladder cancer and make improvements to benefit patients more.

|
Li Xiaoyong Chief of General Surgery Chief Physician
Primary Academic Appointment Trained under the founder of Chinese Hepatobiliary Surgery, Academician Wu Mengchao, the physician graduated from the Medical School of Southeast University in 1986. With nearly 30 years of experience in general surgery, the physician specializes in surgical treatment of difficult liver cancer, hilar cholangiocarcinoma, pancreatic cancer, obstructive jaundice, intrahepatic and extrahepatic bile duct stones, portal hypertension, and abdominal tumors, as well as radiofrequency ablation treatment for liver cancer and postoperative recurrence and metastasis tumors. · Member of the Organ Transplantation Professional Committee of Henan Province · Member of the Liver Cancer Committee of the Henan Anti-Cancer Association · Member of the Hepatic Disease Professional Committee of Henan Province · Member of the Expert Group of the Provincial Medical Accident Appraisal Committee · Editorial board member of several academic journals such as the Henan Journal of Surgery. · In recent years, he has published over 20 national-level professional academic papers and edited or co-edited two professional books. · The physician was the first in the province to introduce and perform precise liver resection techniques, providing a chance for radical surgical resection for some liver cancer patients who were previously considered inoperable. · The physician has won two awards for scientific and technological progress at the municipal and bureau levels, and has been repeatedly recognized as an outstanding doctor, technical star, and medical ethics model in Zhengzhou City. In 2002, the physician was named a top scientific and technological talent at the municipal and bureau levels, and in 2005, 2006, and 2010, was recognized as an advanced individual in the "Three Education" program at Zhengzhou University. · Currently, the physician is undertaking one project at the national level and three projects at the provincial and departmental levels. Hospital Address:Fifth Affiliated Hospital of Zhengzhou University, Zhengzhou. |

|
Chen Yanjun Associate Professor
Primary Academic Appointment Member of the Minimally Invasive Surgery Professional Committee of Henan Province. Graduated from the School of Medicine at Zhengzhou University and has been engaged in general surgery clinical work for 20 years. Has long been responsible for teaching undergraduate and graduate students at Zhengzhou University, serving as a national standardized training instructor for resident physicians and a national training instructor for general practitioners. In 2009, studied liver and gallbladder surgery at the Chinese People's Liberation Army General Hospital (301 Hospital). In recent years, has published more than 10 professional academic papers, co-authored one monograph, participated in one provincial-level project, one project of the National Health and Family Planning Commission, and two provincial-level projects, and has won one provincial-level scientific and technological achievement award. Has a high accuracy rate in the diagnosis of liver, gallbladder, and pancreatic diseases, especially difficult-to-diagnose diseases. Has rich experience and unique insights in surgical treatment and laparoscopic minimally invasive surgery for various benign and malignant liver tumors, complex biliary diseases, biliary tumors, pancreatic tumors, and multidisciplinary comprehensive treatment. Specializes in surgical treatment of hepatobiliary diseases such as primary liver cancer, pancreatic cancer, hilar cholangiocarcinoma, and Budd-Chiari syndrome; laparoscopic minimally invasive surgical treatment of diseases such as gallstones and intrahepatic and extrahepatic bile duct stones. Hospital Address:Fifth Affiliated Hospital of Zhengzhou University, Zhengzhou. |