


Comparative Observation of Irreversible Electroporation and Radioftequency Ablation in Treatment of Liver Cancer was published on Chin J Interv Imaging Ther,2022,vol 19,No 6.
Portions of the article are quoted here to give the reader a more complete understanding of the clinical safety of irreversible electroporation.
【Citation of literature】Li Xueda,YANG Lili,ZHANG Hao,LIU Guoping, Zhang Wei,Li Wei,
LIU Shifeng, WANG Congxiao, WANG Song,HU Xiaokun. Chin J Interv Imaging Ther,2022,vol 19,No 6
Comparative Observation of Irreversible Electroporation and
Radioftequency Ablation in Treatment of Liver Cancer
Li Xueda,YANG Lili,ZHANG Hao,LIU Guoping, Zhang Wei,Li Wei,
LIU Shifeng, WANG Congxiao, WANG Song,HU Xiaokun
[Interventional Medical Center, the Affiliated Hospital of Qingdao University]
Abstract
Objective:To compare the safety and efficacy of irreversible electroporation(IRE)and radiofrequency ablation in treatment of liver cancer.
Methods:Forty-eight patients with liver cancer were prospectively collected and randomly divided into experimental group and control group(each n=24). CT-guided IRE ablation was performed under general anesthesia in experimental group,while CT—guided radiofrequency ablation under local anesthesia was performed in control group.The occurrence of intraoperative and postoperative adverse reactions, and the curative effect were evaluated and compared between groups.
Results:The treatment was successfully completed for both groups of patients, and one case in the trial group died of contrast anaphylaxis, while the rest of patients did not suffer from treatment-related grade 3-4 serious adverse reactions and complications. The differences in the success rates of tumor ablation at 7 days (96.43%, 96.97%), 30 days (96.43%, 93.94%) and 90 days (89.29%, 90.91%) were not statistically significant (P>o.05); the differences in the overall remission rate and disease control rate at each postoperative time point were also not statistically significant (P>o.05).
ConcIusion:IRE ablation had clear efficacy,high safety and light adverse reactions for treatment of liver cancer,with local tumor control effect similar to that of radiofrequency ablation.
Hepatocellular carcinoma is one of the common malignant tumors in clinical practice. Radiofrequency ablation can achieve almost the same effect as surgical resection in the treatment of hepatic malignant nodules, and has been widely used in the clinical mouth, but for tumors adjacent to special areas such as the blood vessels in the hilar region, bile duct, heart, diaphragm or gastrointestinal tract, radiofrequency ablation is susceptible to the "heat sink effect" and has a higher risk of damaging adjacent structures, The risk of local residual tumor and recurrence after treatment is very common. Irreversible electroporation (IRE) ablation is an emerging ablation technique, which can be used for the treatment of liver tumors to effectively preserve blood vessels, bile ducts and other important tissues and their functions in the ablation area. It is a promising alternative to traditional physical ablation for the treatment of liver tumors, which can effectively preserve important tissue structures and their functions. In this study, the efficacy and safety of IRE ablation in the treatment of hepatocellular carcinoma were observed by randomized comparison with radiofrequency ablation.
Treatment Method
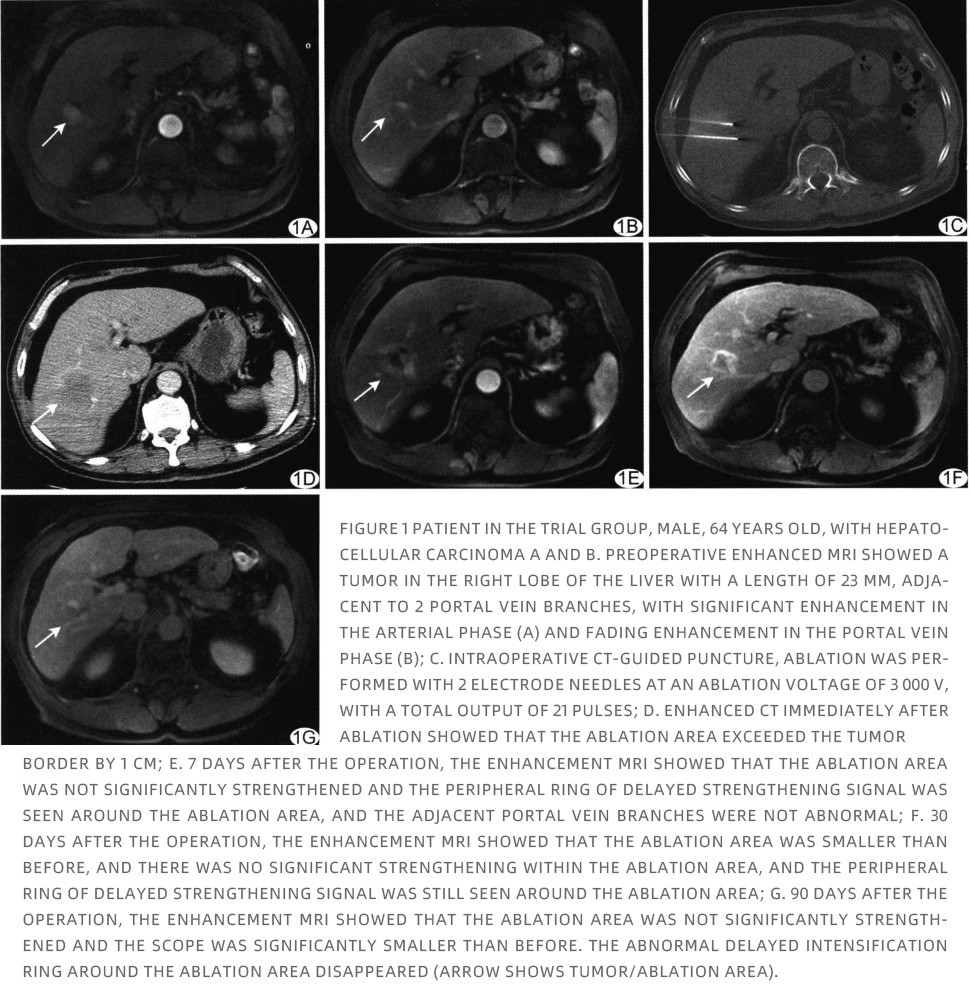
IRE ablation:Patients were fasted for 12 h before the procedure, general anesthesia was administered, sufficient inotropic drugs were given to ensure complete muscle relaxation, and inotropic monitoring and ECG monitoring were performed intraoperatively. The GE Optima620 CT scanner was used as the guidance device to guide the puncture, and 2-4 electrode needles were arranged in parallel at each ablation site. The YTL-GM01 high-voltage steep pulse therapy instrument (Tianjin Yingtai Li'ankang Medical Technology Co., Ltd., now Shanghai Yuanshan Medical Technology Co., Ltd.) was used for ablation, with a voltage of 3000 V and 10-60 sets of output pulses selected according to the size of the cancer site. After ablation, 80 ml of iohexol contrast agent was injected at a flow rate of 3 ml/s through the elbow vein for enhanced CT scan to assess the ablation area, ensure complete ablation of the cancer foci, and observe the changes in the ablation area and complications. See Figure 1.
Radiofrequency ablation:After the skin puncture point and the needle path were determined by CT scan, local anesthesia was administered with 2% lidocaine. The Covidien 11c CTRF 220 radiofrequency ablation system was used to perform radiofrequency ablation under CT guidance; multiple cancer foci were ablated one by one, and multi-point puncture ablation was performed for larger cancer foci. Postoperative enhanced CT scan was performed to clarify the scope of ablation and observe whether there were any complications.
Results
Intraoperative safety:24 cases in the trial group, among which 14 cancer foci were located at special sites, i.e., adjacent to the diaphragm, gallbladder, bile ducts in the hilar region or blood vessels, all successfully completed IRE ablation under general anesthesia without serious adverse effects such as cardiac arrhythmias and blood pressure changes; one case died due to anaphylaxis caused by severe allergy to contrast agent during postoperative enhanced CT examination; the treatment success rate was 100% (23/23). 23). In the control group, 24 cases, including 10 special sites of cancer, were successfully completed with radiofrequency ablation under local anesthesia, and there were no serious adverse reactions and complications during the operation, and the treatment success rate was 100% (24/24).
Laboratory indexes:11 cases in the test group and 9 cases in the control group showed transient impairment of liver function, and the glutathione transaminase increased more than 2 times 7 days after surgery.
Postoperative adverse reactions:There were 4 cases (4/23, 17.39%) of grade 2 adverse reactions in the test group, including 2 cases of pleural effusion, 1 case of abdominal pain and 1 case of fever, and 9 cases (9/24, 37.50%) of grade 2 adverse reactions in the control group, including 8 cases of abdominal pain and 1 case of vomiting, which were completely relieved after symptomatic treatment. no treatment-related grade 3-4 serious adverse reactions and complications occurred in both groups.
Efficacy evaluation:A total of 28 cancer foci were treated with IRE in 23 cases in the test group. 7 days after surgery, 27 (27/28, 96.43%) cancer foci were completely inactivated and 1 had marginal residual activity, i.e. 22 CR and 1 PR; 30 days after surgery, 27 (27/28, 96.43%) cancer foci were completely inactivated and 1 had no change in residual activity, i.e. 22 CR and 1 SD; 90 days after surgery, 25 (25/28, 89.29%) cancer foci were completely inactivated, 1 had increased residual activity and 2 had local recurrence, i.e. 20 CR and 3 PD; At 90 days after surgery, 25 (25/28, 89.29%) cancer foci were completely inactivated, 1 had increased residual activity, and 2 had local recurrence, i.e., 20 CRs and 3 PDs.
In the control group, 24 cases with 33 intrahepatic cancer foci, 7 days after radiofrequency ablation treatment, 32 (32/33, 96.97%) were completely inactivated and 1 still had residual activity, i.e. 23 CR, 1 PR; 30 days after surgery, 31 (31/33, 93.94%) intrahepatic cancer foci had no recurrence (1 intrahepatic lesion was completely inactivated but had iliac metastasis), 1 had no change in residual activity, 1 At 90 days after surgery, 30 (30/33, 90.91%) intrahepatic cancer foci had no recurrence (including 1 case with new intrahepatic foci and 1 case with iliac metastasis), 1 case with increased residual activity, and 2 cases with local recurrence, i.e., 19 cases of CR and 5 cases of PD.
Discussion
The safety and efficacy of IRE ablation for hepatocellular carcinoma have been confirmed by the results of clinical studies at home and abroad, with a technical success rate of 93%, a local recurrence rate of 5%, and tolerated by patients with poor liver function, and postoperative adverse effects mainly include abdominal pain, thoracoabdominal effusion, fever and transient impairment of liver function. The tumor recurrence-free survival rates at 3, 6 and 12 months after surgery were 87.4%, 78.4% and 74.8%, respectively, but the incidence of severe complications was 11.5%, mainly including liver abscess, portal vein thrombosis, abdominal hemorrhage and cardiovascular-related complications. In this study, one patient in the experimental group died of contrast allergy, but the rest of patients did not have serious complications. The success rate of IRE ablation for tumor treatment was 96.43%, and the local recurrence-free rates 30 and 90 days after surgery were 96.43% and 89.29%, respectively, which were not significantly different from those of the control group, suggesting that IRE ablation for liver cancer is safe and its efficacy is comparable to that of radiofrequency ablation.
There are many factors affecting the efficacy of IRE ablation, and the size and location of the tumor are the main influencing factors. Accurate puncture positioning and determining the effective ablation range are the keys to ensure complete local ablation. According to the preoperative CT images, combined with the multilevel reconstruction images, the electrode needles should be parallel to each other as much as possible to avoid the uneven distribution of electric field, and the enhanced CT scan immediately after ablation can help to clarify the actual ablation boundary and ensure that the ablation range exceeds the tumor boundary by more than 1 cm to avoid tumor residue. The success rate of IRE ablation was 91.4%, and there were no serious complications associated with it. In this study, 14 cancer foci in the experimental group and 10 cancer foci in the control group were located in special sites, which benefited from the reasonable selection of ablation parameters and effective control of the ablation range, and no serious adverse effects and complications occurred. In the test group, one cancer site adjacent to the diaphragm and right hepatic vein had residual activity and a moderate amount of pleural effusion after surgery, while the rest of the cancer sites were completely inactivated; in the control group, one cancer site at a special location had residual activity 7 days after surgery and one recurrence 90 days after surgery. The tumor located in the special site is still an important factor affecting the effect of ablation treatment.
In conclusion, IRE ablation for hepatocellular carcinoma is safe, reliable, and has clear efficacy. Combined with general intravenous anesthesia and effective muscarinic treatment, it can significantly reduce the risk of surgery; the local tumor control effect is comparable to that of radiofrequency ablation treatment, which can be used as an alternative option and has obvious advantages for tumors in special sites. However, the sample size of this study is limited, and the individual differences of grade 1-2 adverse reactions are large, so the data of grade 2 adverse reactions were not compared, and further observation is needed.

Li Xue Da Chief Physician, Master's Degree
Primary Academic Appointment He is mainly engaged in basic and clinical research of interventional treatment of malignant tumors. His clinical experience includes chemoembolization of malignant tumors, interventional treatment of obstructive jaundice, interventional thrombolysis and angioplasty of visceral and extremity vascular stenosis, embolization of acute bleeding, interventional treatment of peripheral vascular malformation, peripheral vascular stenosis, cerebral vascular stenosis and aneurysm, etc. He has accumulated rich clinical experience in non-vascular interventional treatment such as radiofrequency ablation of various solid tumors, I125 particle implantation and argon helium knife freezing. He has accumulated rich clinical experience in non-vascular interventions such as radiofrequency ablation, I125 particle implantation and Ar-He knife freezing for various solid tumors. Specialty expertise Chemoembolization of malignant tumors; interventional treatment of obstructive jaundice; interventional thrombolysis and angioplasty of visceral and extremity vascular stenosis; embolization treatment of various acute bleeding; interventional treatment of peripheral vascular malformation, peripheral vascular stenosis, cerebral vascular stenosis and aneurysm. |
Currently, a multi-center clinical registration trial of the Steep Pulse Therapeutic Apparatus (Nanoknife) for the ablation treatment of pancreatic malignant tumors is underway in several hospitals across the country. For more information, please leave a message in the background or contact the following person by phone.
Contact person:Manage Zuo from Alpmed
Tel:022-23788188 Ext 7206